Friday, July 31, 2009
Tuesday, July 28, 2009
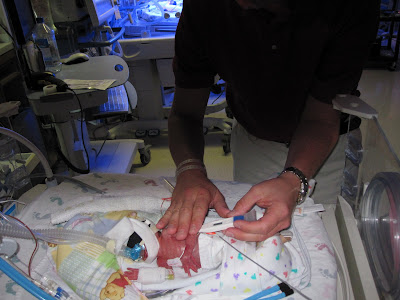
Kangaroo Care
The last two days have been thrilling, with being able to hold the girls. The style of holding we are doing is called Kangaroo Care. Kangaroo Care is a way of holding a preterm infant so that there is skin-to-skin contact between the infant and the person holding it. The baby, wearing only a diaper, is held against the parent's bare chest. Researchers have found that the close physical contact with the parent can help to stabilize the preterm infant's heartbeat, temperature, and breathing. Preterm infants often have difficulty coordinating their breathing and heart rate. Researchers also have found that mothers who use kangaroo care often have more success with breastfeeding and improve their milk supply. Further, researchers have found that preterm infants who experience kangaroo care have longer periods of sleep, gain more weight, decrease their crying, have longer periods of alertness, and earlier hospital discharge.
So now you know if you see one of us is a hospital gown, or Mikes old ugly shirt :) in a lot of pictures, it is so the girls can lay flush with our skin. Hopefully as they get stronger and healthier the amount of Kangaroo Care will be able to increase.
So now you know if you see one of us is a hospital gown, or Mikes old ugly shirt :) in a lot of pictures, it is so the girls can lay flush with our skin. Hopefully as they get stronger and healthier the amount of Kangaroo Care will be able to increase.
Monday, July 27, 2009
The beginning of our experience…
We just wanted to step back for a second and recap our experience that lead up to the birth of Jenna and Abigail.
Once Upon a Time…
After toying with the idea of taking one last big vacation before we became parents, we decided just to spend a few days in Hermann, Staying at our favorite Bed and Breakfast Hermann Hill for their “babymoon” package, Wednesday and Thursday nights (15th and 16th of July).
Thursday afternoon, Leah started to feel just a little bit off, and had called into her doctor’s office who said that her symptoms didn’t sound problematic, and to just take it easy, which she did, after all, we were on vacation. So, after a beautiful day of Mike drinking wine and Leah enjoying the sights of Hermann, we had dinner at Stone Hill and went back for a good nights rest at our Bed and Breakfast.
Well, it did not end up being a good night’s sleep – Leah woke up not feeling quite right. We ended up leaving right after finishing up breakfast. As we got back to St. Louis, Leah started having some weird cramping. Becoming even more concerned, we decided to go straight to St. John’s rather than wait a few more hours for her to see her doctor at the office.
We arrived at St. John’s and went directly to the Women’s Evaluation Unit. After about 15 minutes we were moved into an examination room where a nurse/midwife began going through the routine checks to see how Leah was doing. She put some sensors on Leah to check for contractions, very shortly into her exam she stood up with a panicked look on her face. She had found that Leah was already dilated 3 ½ centimeters with part of Baby A’s amniotic sac bulging out.
Immediately we were taken to Labor and Delivery. We were at 23 weeks and 6 days, not due until November 7th. While we had expected them to be early, this was a bit more than we had ever planned for – our childbirth classes weren’t even supposed to start until that Tuesday. At L&D, we were met with many nurses and doctors, including a visit from a doctor from the Neonatal Intensive Care Unit (NICU). We were told that babies born at 24 weeks, across all births, have about a 50% chance at survival, as full gestation is 40 weeks. As scary as that was, we knew were in one of the best places possible if the girls were going to be impatient and come as early as it looked might happen.
The good thing was that Leah’s water had not broken. That meant that if they could slow the contractions down, she could remain at L&D for as long as needed. At that point though, we knew she would not be going back home still pregnant. It could have been that night, that week, or even a month away. Every day was an achievement, and gave the girls a better chance. Most importantly, we were told, was to make it at least 48 hours so that a series of steroid injections Leah would be given would have the greatest impact on helping the girls lungs develop, so they would have a better chance when they did arrive. Leah was having contractions every 4-6 minutes and was dilated 3-4 cm. How would we ever make 48 hours? We were told even 12 hours would be important, as well as every 12 hours after that.
So there we were, at L&D at St. Johns, trying to keep the girls in as long as possible.
Leah was immediately confined to her bed. Her home for the next hours/days/weeks was going to be a labor and delivery bed. She was put into the trendelenberg position with her feet several inches higher than her waist and her head several inches lower, in an effort to put less stress on the amniotic sac. She was also given a mixture of drugs to slow down her contractions, and to try to keep her pregnant for as long as possible.
Late that afternoon, Leah was having contractions at a rate of one every 2-3 minutes. The perinatologist had a very aggressive plan. The main drug they were giving her was an IV drip of Magnesium Sulfate. They usually give you an initial dose of mag, then a maintenance level to keep things at a certain level. Leah ended up getting two initial doses, and then was maintained at the highest possible level.
Leah’s contractions slowed a bit into the evening, maybe one ever 10 minutes or so, but they were becoming stronger. Once or twice she crushed Mike’s hand during a contraction, until her dad bought her a squishy air filled stress ball (which only had air in it for an hour or so, but ended up working just fine deflated).
Friday night ended up being a long night for the both of us. Leah was having contractions ever 15 minutes and couldn’t sleep. Nurses were in a few times an hour. Mike was resting in a recliner next to Leah’s bed, but not getting much sleep either with everything that was going on.
On Saturday morning, many of the faces we saw during the day before were back in L&D. They had gone home after their shift at 7pm the night before not expecting to see Leah still there, and still pregnant when they came in the next day. But there she was, still in the same room, with two little girls still inside her. She was still having strong contractions, but they were now maybe once or twice an hour. Amazingly, she had not dilated any further.
As Saturday progressed, Leah’s contractions became slower and slower, but were still fairly strong. It was a long day, but we were grateful to have the support of our family there with us, taking shifts to keep Leah company so Mike could run home and feed the cats and get a bit of rest for himself. The mag starting really having an effect on Leah, the thermostat in the room was set as cold as possible, the ceiling fan was on full blast, and two other fans were brought in and pointed directly at Leah, yet she continued to not cool down. Everyone else was covered in blankets and coats, and Leah in her hospital gown was still sweating. Some of the other effects from the drugs started to set in. Leah began not to be able to move her arms and legs, and her thinking was muddled, confused, and cloudy.
However, Saturday passed by and we had made it to 24 hours +. It seemed like things were headed in the right direction. Maybe things could get settled down, we could get some rest, and maybe dig in for a long stay at St. Johns. Saturday night ended up being a bit rough on Leah. Sleep was difficult, as the drugs caused vivid and scary dreams, not to mention the endless but needed nurse interruptions. At this point it had also been a day and a half of only being allowed small sips of water when taking meds, and not having a bite to eat, not that she had any appetite at that point.
Sunday morning, after an hour or two of sleep, we “woke” up. It was a good day because Leah was still pregnant. Sunday at 3pm was our goal – 48 hours after the steroids to help out the girls lungs. It seemed like a very real possibility at that point, and maybe even more. Leah’s contractions were down to about once every 60-90 minutes, and they weren’t nearly as strong as they had been.
Sunday passed by, and it seemed like a relatively uneventful day. Leah’s contractions were getting slower and slower and continuing to get lighter as well. 48 hours passed, and now we were in bonus territory. We got the two big days and every extra day was still very important, but not as critical as the initial 48. Although the physical effects from the mag were ever increasing, and at this point Leah could only move her toes and fingers. Leah also began having mild hallucinations, and began to become confused as to what was imaginary and what was reality.
Early Sunday evening Leah began to feel a pressure in her chest, this was an indicator that she had developed fluid in her lungs. Blood was drawn, and it showed that the mag levels in Leah’s system were high, but still within theriputic boundaries. As a precaution, they decided to turn the mag off for an hour to help her lungs try and get some of the fluid out. As 2am rolled around, Leah woke up. It was excruciating to breathe, she felt like she drowning. It also felt as if she had a load of bricks on her chest,. We rang the nurses, they gave her O2, then gave her more, then gave her an O2 mask. It was a combination of the mag that she had been for 60 hours now and being in the trendelenberg position (or “upsidedown”) for nearly three days. Her lungs were taking on fluid because her lungs and heart could not push the fluid away like they needed to. Her blood was drawn, and she had hit the ceiling for mag levels in her system. She was taken off the mag, taken out of the trendelenberg position and was started on lasics to remove the excess fluids. Over the next hour her breathing improved slightly, and slowly throughout the following day her breathing continued to gradually improve. All the other effects from the mag began to dissipate as well.
On Monday Leah was going to start taking another drug to try and maintain her reduced contraction rate and level. For a third day, her contractions continued to slow, now once every 2-3 hours. No one usually wants to be in the hospital for a really long time, but we were happy to be there as long as we could. By now, Leah’s lungs were feeling a bit better, and she finally got a meal to eat. As it now looked we might be here a while, we were trying to get a normal routine started. Mike went into work late to get caught up while family took turns keeping Leah company at St. Johns. It was shaping up to be an uneventful day. Maybe finally, we would get some sleep…
A few hours into Monday night, Leah started having more frequent contractions again. 30 minutes, then 20 minutes, then about 10-15 minutes. Nurses were in frequently to check up on her. From 3-4 am, she was having them every 5-6 minutes. Leah felt something different, she just knew something wasn’t right. The ultrasound was done around 4:30. Mike had seen them scan Leah several times over the last few days as they checked how far she was dilated and knew what it looked like. He knew even before the resident said anything – there was something in the area that had been a dark spot each and every time before over the last few days. Baby A’s feet were now coming through the cervix. We would soon be headed to the OR for Leah to have an emergency caesarean section. What we originally didn’t expect to happen until October was going to happen very soon. We were about to meet our daughters. It was July 21st.
Besides Leah’s continuing need for oxygen, and the two teams from the NICU standing by, it was a fairly routine c-section. As each baby was born, they were rushed into the waiting hands of a NICU team, we heard each of them cry, and it was the most beautiful sound we had ever heard. They were quickly stabilized, introduced to Mommy and Daddy and taken to the NICU, where they will remain for months of hard work and growing. They are truly remarkable little miracles.
Immediately after their birth Leah felt a relief in her lungs. Although in the days ahead, she developed pneumonia, and heartbreakingly could not visit the girls until her fever cleared. Mike took many trips to the NICU bringing back pictures and video to share until she was able to visit again on Friday.
We are both truly grateful for the care Leah received and that Jenna and Abigail continue to receive at St. John’s. The nurses and support staff have just been incredible, going above and beyond to make the best of a very harrowing experience. We could not have asked for anything more.
We would also like to thank our families for their unwavering support, love, and commitment. We don’t think that we could have gotten through this without them.
Once Upon a Time…
After toying with the idea of taking one last big vacation before we became parents, we decided just to spend a few days in Hermann, Staying at our favorite Bed and Breakfast Hermann Hill for their “babymoon” package, Wednesday and Thursday nights (15th and 16th of July).
Thursday afternoon, Leah started to feel just a little bit off, and had called into her doctor’s office who said that her symptoms didn’t sound problematic, and to just take it easy, which she did, after all, we were on vacation. So, after a beautiful day of Mike drinking wine and Leah enjoying the sights of Hermann, we had dinner at Stone Hill and went back for a good nights rest at our Bed and Breakfast.
Well, it did not end up being a good night’s sleep – Leah woke up not feeling quite right. We ended up leaving right after finishing up breakfast. As we got back to St. Louis, Leah started having some weird cramping. Becoming even more concerned, we decided to go straight to St. John’s rather than wait a few more hours for her to see her doctor at the office.
We arrived at St. John’s and went directly to the Women’s Evaluation Unit. After about 15 minutes we were moved into an examination room where a nurse/midwife began going through the routine checks to see how Leah was doing. She put some sensors on Leah to check for contractions, very shortly into her exam she stood up with a panicked look on her face. She had found that Leah was already dilated 3 ½ centimeters with part of Baby A’s amniotic sac bulging out.
Immediately we were taken to Labor and Delivery. We were at 23 weeks and 6 days, not due until November 7th. While we had expected them to be early, this was a bit more than we had ever planned for – our childbirth classes weren’t even supposed to start until that Tuesday. At L&D, we were met with many nurses and doctors, including a visit from a doctor from the Neonatal Intensive Care Unit (NICU). We were told that babies born at 24 weeks, across all births, have about a 50% chance at survival, as full gestation is 40 weeks. As scary as that was, we knew were in one of the best places possible if the girls were going to be impatient and come as early as it looked might happen.
The good thing was that Leah’s water had not broken. That meant that if they could slow the contractions down, she could remain at L&D for as long as needed. At that point though, we knew she would not be going back home still pregnant. It could have been that night, that week, or even a month away. Every day was an achievement, and gave the girls a better chance. Most importantly, we were told, was to make it at least 48 hours so that a series of steroid injections Leah would be given would have the greatest impact on helping the girls lungs develop, so they would have a better chance when they did arrive. Leah was having contractions every 4-6 minutes and was dilated 3-4 cm. How would we ever make 48 hours? We were told even 12 hours would be important, as well as every 12 hours after that.
So there we were, at L&D at St. Johns, trying to keep the girls in as long as possible.
Leah was immediately confined to her bed. Her home for the next hours/days/weeks was going to be a labor and delivery bed. She was put into the trendelenberg position with her feet several inches higher than her waist and her head several inches lower, in an effort to put less stress on the amniotic sac. She was also given a mixture of drugs to slow down her contractions, and to try to keep her pregnant for as long as possible.
Late that afternoon, Leah was having contractions at a rate of one every 2-3 minutes. The perinatologist had a very aggressive plan. The main drug they were giving her was an IV drip of Magnesium Sulfate. They usually give you an initial dose of mag, then a maintenance level to keep things at a certain level. Leah ended up getting two initial doses, and then was maintained at the highest possible level.
Leah’s contractions slowed a bit into the evening, maybe one ever 10 minutes or so, but they were becoming stronger. Once or twice she crushed Mike’s hand during a contraction, until her dad bought her a squishy air filled stress ball (which only had air in it for an hour or so, but ended up working just fine deflated).
Friday night ended up being a long night for the both of us. Leah was having contractions ever 15 minutes and couldn’t sleep. Nurses were in a few times an hour. Mike was resting in a recliner next to Leah’s bed, but not getting much sleep either with everything that was going on.
On Saturday morning, many of the faces we saw during the day before were back in L&D. They had gone home after their shift at 7pm the night before not expecting to see Leah still there, and still pregnant when they came in the next day. But there she was, still in the same room, with two little girls still inside her. She was still having strong contractions, but they were now maybe once or twice an hour. Amazingly, she had not dilated any further.
As Saturday progressed, Leah’s contractions became slower and slower, but were still fairly strong. It was a long day, but we were grateful to have the support of our family there with us, taking shifts to keep Leah company so Mike could run home and feed the cats and get a bit of rest for himself. The mag starting really having an effect on Leah, the thermostat in the room was set as cold as possible, the ceiling fan was on full blast, and two other fans were brought in and pointed directly at Leah, yet she continued to not cool down. Everyone else was covered in blankets and coats, and Leah in her hospital gown was still sweating. Some of the other effects from the drugs started to set in. Leah began not to be able to move her arms and legs, and her thinking was muddled, confused, and cloudy.
However, Saturday passed by and we had made it to 24 hours +. It seemed like things were headed in the right direction. Maybe things could get settled down, we could get some rest, and maybe dig in for a long stay at St. Johns. Saturday night ended up being a bit rough on Leah. Sleep was difficult, as the drugs caused vivid and scary dreams, not to mention the endless but needed nurse interruptions. At this point it had also been a day and a half of only being allowed small sips of water when taking meds, and not having a bite to eat, not that she had any appetite at that point.
Sunday morning, after an hour or two of sleep, we “woke” up. It was a good day because Leah was still pregnant. Sunday at 3pm was our goal – 48 hours after the steroids to help out the girls lungs. It seemed like a very real possibility at that point, and maybe even more. Leah’s contractions were down to about once every 60-90 minutes, and they weren’t nearly as strong as they had been.
Sunday passed by, and it seemed like a relatively uneventful day. Leah’s contractions were getting slower and slower and continuing to get lighter as well. 48 hours passed, and now we were in bonus territory. We got the two big days and every extra day was still very important, but not as critical as the initial 48. Although the physical effects from the mag were ever increasing, and at this point Leah could only move her toes and fingers. Leah also began having mild hallucinations, and began to become confused as to what was imaginary and what was reality.
Early Sunday evening Leah began to feel a pressure in her chest, this was an indicator that she had developed fluid in her lungs. Blood was drawn, and it showed that the mag levels in Leah’s system were high, but still within theriputic boundaries. As a precaution, they decided to turn the mag off for an hour to help her lungs try and get some of the fluid out. As 2am rolled around, Leah woke up. It was excruciating to breathe, she felt like she drowning. It also felt as if she had a load of bricks on her chest,. We rang the nurses, they gave her O2, then gave her more, then gave her an O2 mask. It was a combination of the mag that she had been for 60 hours now and being in the trendelenberg position (or “upsidedown”) for nearly three days. Her lungs were taking on fluid because her lungs and heart could not push the fluid away like they needed to. Her blood was drawn, and she had hit the ceiling for mag levels in her system. She was taken off the mag, taken out of the trendelenberg position and was started on lasics to remove the excess fluids. Over the next hour her breathing improved slightly, and slowly throughout the following day her breathing continued to gradually improve. All the other effects from the mag began to dissipate as well.
On Monday Leah was going to start taking another drug to try and maintain her reduced contraction rate and level. For a third day, her contractions continued to slow, now once every 2-3 hours. No one usually wants to be in the hospital for a really long time, but we were happy to be there as long as we could. By now, Leah’s lungs were feeling a bit better, and she finally got a meal to eat. As it now looked we might be here a while, we were trying to get a normal routine started. Mike went into work late to get caught up while family took turns keeping Leah company at St. Johns. It was shaping up to be an uneventful day. Maybe finally, we would get some sleep…
A few hours into Monday night, Leah started having more frequent contractions again. 30 minutes, then 20 minutes, then about 10-15 minutes. Nurses were in frequently to check up on her. From 3-4 am, she was having them every 5-6 minutes. Leah felt something different, she just knew something wasn’t right. The ultrasound was done around 4:30. Mike had seen them scan Leah several times over the last few days as they checked how far she was dilated and knew what it looked like. He knew even before the resident said anything – there was something in the area that had been a dark spot each and every time before over the last few days. Baby A’s feet were now coming through the cervix. We would soon be headed to the OR for Leah to have an emergency caesarean section. What we originally didn’t expect to happen until October was going to happen very soon. We were about to meet our daughters. It was July 21st.
Besides Leah’s continuing need for oxygen, and the two teams from the NICU standing by, it was a fairly routine c-section. As each baby was born, they were rushed into the waiting hands of a NICU team, we heard each of them cry, and it was the most beautiful sound we had ever heard. They were quickly stabilized, introduced to Mommy and Daddy and taken to the NICU, where they will remain for months of hard work and growing. They are truly remarkable little miracles.
Immediately after their birth Leah felt a relief in her lungs. Although in the days ahead, she developed pneumonia, and heartbreakingly could not visit the girls until her fever cleared. Mike took many trips to the NICU bringing back pictures and video to share until she was able to visit again on Friday.
We are both truly grateful for the care Leah received and that Jenna and Abigail continue to receive at St. John’s. The nurses and support staff have just been incredible, going above and beyond to make the best of a very harrowing experience. We could not have asked for anything more.
We would also like to thank our families for their unwavering support, love, and commitment. We don’t think that we could have gotten through this without them.
Subscribe to:
Posts (Atom)